In stage 4 melanoma, the cancer has spread from its place of origin to other parts of the body, such as the lungs, brain, liver, spinal cord, bone, digestive tract, soft tissue, and distant lymph nodes.
Melanoma occurs when the pigment-producing cells called melanocytes mutate and become cancerous.
Stage 4 melanoma, also called metastatic melanoma, occurs when cancer cells have traveled through the blood or lymphatic system to other parts of the body.

According to the
The Memorial Sloan Kettering Cancer Center (MSKCC) suggests that the survival rate has increased to 50% due to newer treatment options.
It is important to note that many factors influence an individual’s chance of survival. Survival rates are estimates based on data from large group studies that do not consider individual circumstances.
People’s age and their response to treatment can affect survival rates, as well as the availability of new treatment options.
Is stage 4 melanoma curable?
According to the MSKCC, newer treatment options can control advanced melanoma for years and even cure it.
A 2024 article notes that treatment with checkpoint inhibitors, which are a type of immunotherapy, offers the best chances of curing advanced melanoma.
Melanoma can develop on any part of the body but is more likely to affect the chest, back, legs, neck, and face. This can vary depending on a person’s race, gender, and age.
The American Academy of Dermatology states that melanoma develops more often on the legs in females, and males tend to develop melanomas more commonly on the torso, head, and neck.
People with skin of color are more likely to develop melanoma on the parts of the body that have less sun exposure, such as:
- the soles
- the palms
- the groin
- the inside of the mouth
- under the nails
The
Other symptoms of stage 4 melanoma include:
- a sore that does not heal
- skin discoloration or swelling beyond the border of the mole
- itching, tenderness, or pain
- scaling, oozing, bleeding, or a change in the surface of the mole, lump, or bump
Swollen or hard lymph nodes are another sign. A doctor can confirm this by performing a physical examination. Other tests include blood tests and imaging scans to confirm the presence of cancer and check the extent of its spread.


Warning
Contains Sensitive Content
Warning
Contains Sensitive Content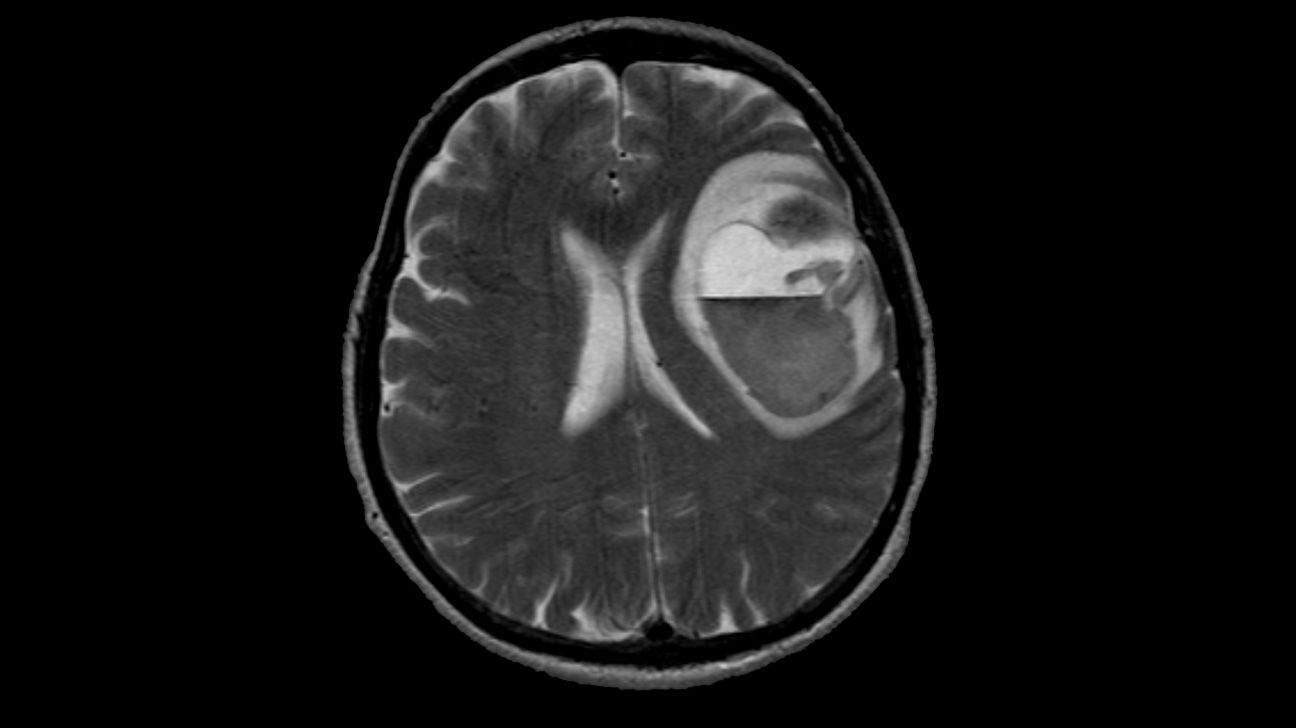

Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive Content
Warning
Contains Sensitive ContentA healthcare professional may suggest immunotherapy with checkpoint inhibitors and targeted drugs to treat widespread melanoma.
The first treatment option includes checkpoint inhibitors. Options include:
- pembrolizumab or nivolumab
- nivolumab with relatlimab
- nivolumab or pembrolizumab, with ipilimumab
About
If checkpoint inhibitors are not working, other immunotherapy drugs can include interleukin-2 or lifileucel.
Chemotherapy can also help treat some people with stage 4 melanoma. If chemotherapy is necessary, a healthcare professional may recommend the chemotherapy drugs dacarbazine and temozolomide.
People who do not respond to current treatments can also consider enrolling in clinical trials. These studies continue to look for new targeted drugs and combinations of treatments that can improve cancer care and quality of life.
People can do a few things to make it easier to cope with a stage 4 melanoma diagnosis, the treatment, and the post-treatment journey:
- Keep all follow-up appointments: It is vital to see a doctor frequently to discuss any side effects and check for new signs of melanoma. People with advanced-stage melanomas should have physical exams every
3 to 6 monthsTrusted Source for several years, even after completing treatment. - Seek out emotional support: Some people may have anxiety, while others experience feelings of denial, anger, and depression. A person may benefit from speaking openly about these feelings and seeking help from loved ones, support groups, and therapists.
- Consult a nutrition expert or lifestyle counselor: Eating a balanced diet and increasing physical activity levels can aid recovery and improve long-term health.
It is natural to have questions about the treatment, its side effects, and the chances of cancer recurring. People with concerns should discuss them with a doctor who can offer advice about their medical history and overall health.
Stage 4 melanoma, or metastatic melanoma, occurs when the cancer cells spread through the blood or lymphatic system to more distant parts of the body.
Anyone with stage 4 melanoma diagnosis should speak with a doctor frequently about their symptoms and reach out to loved ones and professionals for emotional support.

